UM, PARDON ME?
I've been seeing a lot of questions lately in my office and online about "queefing". Whomever came up with the term queefing, in my humble opinion, is an absolute genius! So, what exactly is the definition of queefing? According to Dictionary.com:
NOUN: Slang: Vulgar. an expulsion of air through the vagina.
Queefing FAQs
Since there seems to be a lot of confusion about queefing, so let's tackle the most common questions.
How common is queefing?
In the general population, we just don't know for sure. One literature review, says it's between 1 and 69%. The single article I could locate on the topic of prevalence found that 69% of women pass gas via the vagina at least twice a week. Let's go with 69% as the best number we've got. Asking around my office and my female friends, most women will admit they've queefed before, even if it isn't a regular problem.How does the air get in there?
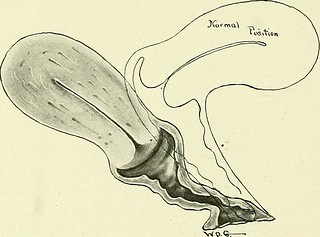
Vaginal air can come from two places. First, it can get in the vagina from something called a fistula. A fistula is a little opening between the bowel and the vagina, most often seen after traumatic prolonged vaginal delivery, or after vaginal/pelvic surgery. This can be diagnosed in your doctor's office or with imaging, like a CT or MRI.Does a queef smell bad?
 If a man farts in the forest, and no one is there to appreciate it, does it smell? Depends on how you think about it. In order for something to smell, a nose must be there to inhale the chemicals that produce a signal in the brain of a particular odor. When you pass flatus (that's the actual medical term for rectal gas) most of the time it has little or no odor. Rectal gas is a combination of swallowed air and byproducts of the microbes living in your gut. Certain foods notorious for gas (like broccoli and milk) are partly broken down by bacteria in your gut, which produces hydrogen sulfide. That chemical is what gives smelly farts their odor.
If a man farts in the forest, and no one is there to appreciate it, does it smell? Depends on how you think about it. In order for something to smell, a nose must be there to inhale the chemicals that produce a signal in the brain of a particular odor. When you pass flatus (that's the actual medical term for rectal gas) most of the time it has little or no odor. Rectal gas is a combination of swallowed air and byproducts of the microbes living in your gut. Certain foods notorious for gas (like broccoli and milk) are partly broken down by bacteria in your gut, which produces hydrogen sulfide. That chemical is what gives smelly farts their odor.
 Is queefing dangerous?
Is queefing dangerous?
Nope. Not in the least. If it's associated with a fistula, it'll need to be fixed. But classic passage of vaginal air that's trapped is common, and normal. It doesn't hurt, and is not dangerous. But it can be embarrassing. Many times a queef makes a noise similar to a fart. That sound can draw attention, obviously, and women with regular queefs tend to feel shameful about it.
Is there anything I can do to reduce or stop it?
There's no literature on this. These recommendations come from experience and from a little medical logic. If you queef mostly after sex, using a good lubricant can help. When the penis slides more easily, it doesn't push as much air up in there. Good lubricants are generally either water or silicone based. You'll need to use one that's pH balanced. The lubricants I recommend to my patients are "Good Clean Love", "Desert Harvest Glide", and "Uberlube". If you're one that queefs after sitting too long at work, getting up regularly will reduce the likelihood of having the sound.What's next?
If you queef more than twice a week, you may have a pelvic floor issue. You can always come by my office to talk about the sensitive topics like this. We'll figure out if your queefs are concerning or just the garden variety "gentle wind". You can make an appointment with me at Nurture Womens Health.
https://www.ncbi.nlm.nih.gov/pubmed/28494270
https://www.ncbi.nlm.nih.gov/pubmed/26241266
https://www.ncbi.nlm.nih.gov/pubmed/14677001