How Pain Works
 All pelvic pain patients have several things in common. Pain starts in the body, gets sent up the spinal cord, and gets processed in the brain. This happens in every single person. It's kind of like a relay race. If the baton doesn't get passed, or if someone poops out and stops running, the baton never makes it to the finish line. Without a pain signal or the ability to relay and process it, you wouldn’t have pain. Think about people with spinal cord injuries and paralysis. Paralyzed people can’t feel pain below their injury. The pain signals are still there, but they can’t get to the brain. The pain doesn’t get past the injury in the spine. No relay, no pain.
All pelvic pain patients have several things in common. Pain starts in the body, gets sent up the spinal cord, and gets processed in the brain. This happens in every single person. It's kind of like a relay race. If the baton doesn't get passed, or if someone poops out and stops running, the baton never makes it to the finish line. Without a pain signal or the ability to relay and process it, you wouldn’t have pain. Think about people with spinal cord injuries and paralysis. Paralyzed people can’t feel pain below their injury. The pain signals are still there, but they can’t get to the brain. The pain doesn’t get past the injury in the spine. No relay, no pain. Pain Tolerance
Once the pain makes it all the way to the brain, it has to be processed. This is where things get even more interesting. There are multiple studies that show that patients with chronic pain have a different tolerance for pain. If you took a person without a pain condition and laid them down in an MRI machine, it would take something pretty noxious, like poking them with a sharp object to see a lighting up of the pain centers in the brain. In pelvic pain patients, the MRI shows the pain centers lighting up much easier, like with normal touch, or sometimes even just light touch with a cotton swab! Everyone’s tolerance for lighting up the pain centers is a little different.
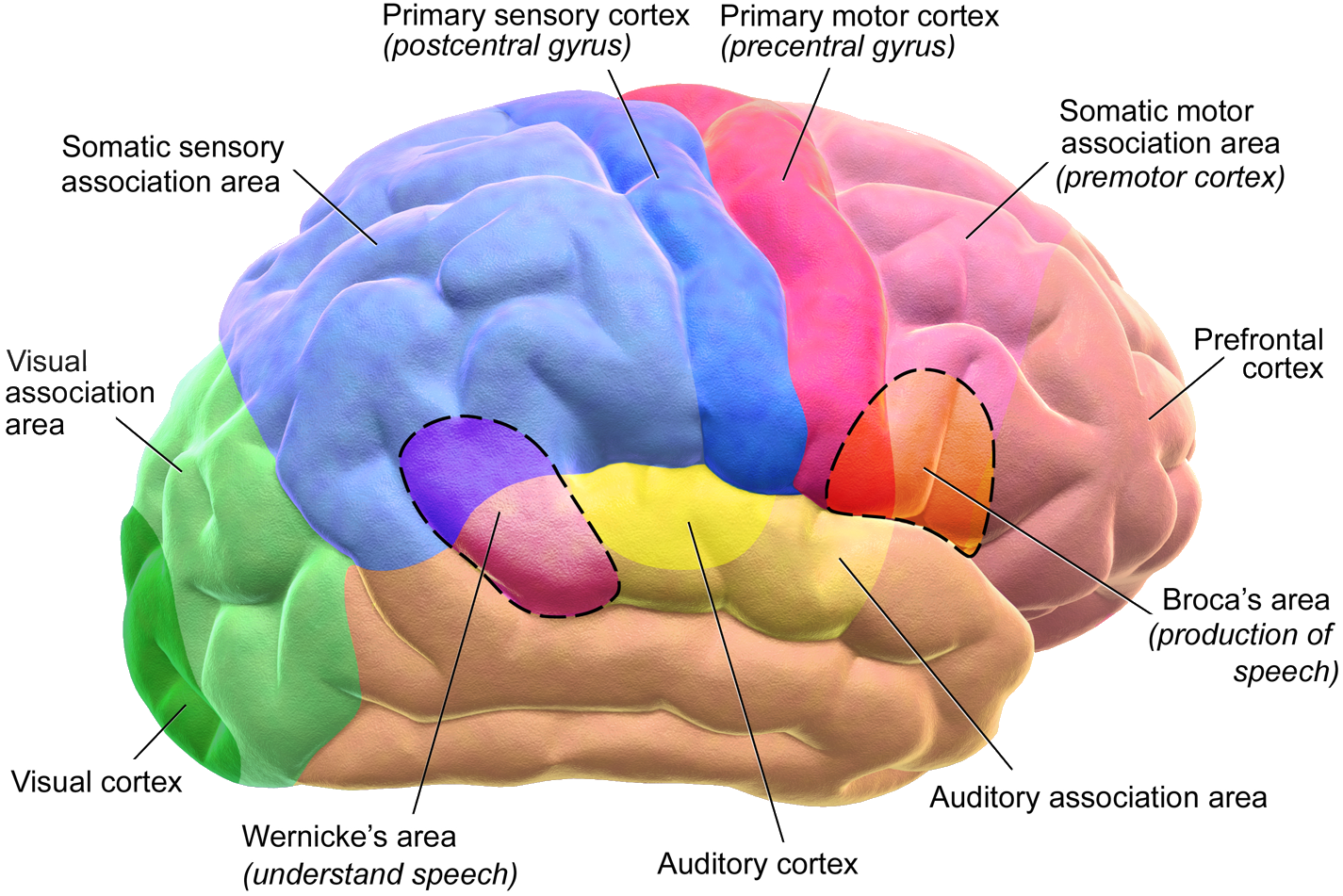
All pain is processed in the same areas of the brain. Science doesn’t have this completely figured out yet, but we do know that pain signals go through certain pathways, hitting certain areas for processing. As the pain is processed, it’s localized and given meaning and context. The same mixture of chemicals are released when you’re riding a rollercoaster and when you’re being chased by a bear. How does the brain know which one is fun and which one is scary?
By knowing which areas are being used for processing, we can figure out what to do to interfere with that part of the process and make more pleasure and less pain. All pain is also modifiable by changing the circumstances of the pain and its surroundings.
Pain Processing Centers
All pain is processed in the same areas of the brain. Science doesn’t have this completely figured out yet, but we do know that pain signals go through certain pathways, hitting certain areas for processing. As the pain is processed, it’s localized and given meaning and context. The same mixture of chemicals are released when you’re riding a rollercoaster and when you’re being chased by a bear. How does the brain know which one is fun and which one is scary?
By knowing which areas are being used for processing, we can figure out what to do to interfere with that part of the process and make more pleasure and less pain. All pain is also modifiable by changing the circumstances of the pain and its surroundings.